Optimal Stopping in Radiotherapy
Although radiation therapy (RT) is one of the main curative modalities in cancer treatment, unfortunately in some patients it is not effective in curbing cancer progression. This is mainly due to the differences in tumor's and patient's overall biological makeup which makes the tumor cells extremely radioresistant. In such cases, continuation of the treatment course might not only be harmful for patients (due to the radiation-induced damage to healthy tissues), but, due to the prolonged nature of most RT treatment courses, might prevent from undertaking a more effective treatment option. Therefore, it is highly desirable to identify those patients for whom RT might not be the best course of action, and stop the treatment immediately. This problem can be formulated as a special case of Optimal Stopping problem. We have termed this Optimal Stopping in Radiation Therapy (OSRT) [1].
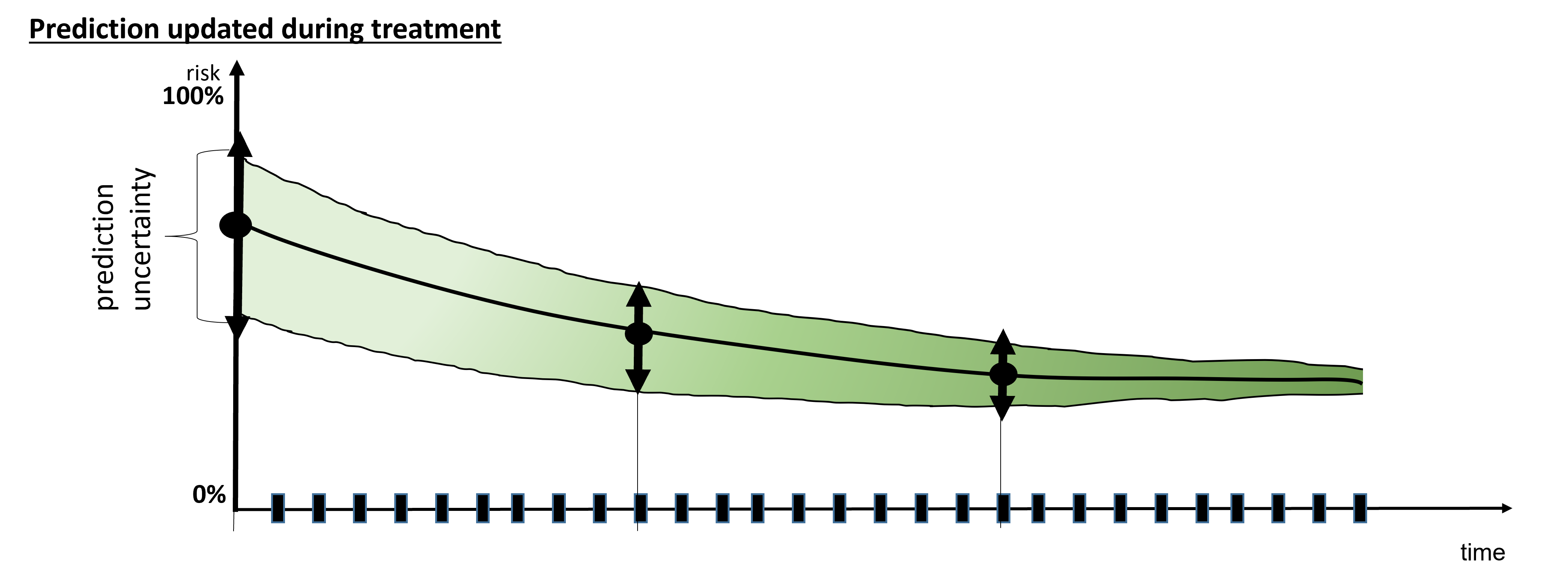
OSRT can be seen as a special case of the broader personalized medicine, in which the treatment course is adapted based on individual's biological characteristics. Owing to the recent advancements in functional imaging and micro-array analysis, more patient-specific data is available before, during, and after the treatment. The crux of the problem is how to integrate this extremely complex, heterogeneous, and noisy data into a panoptic view of the patient's response landscape. The idea is to view the patient response to RT as a stochastic problem whose states (i.e., tumor progression, normal tissue damage) stochastically evolve during and after the course of the treatment, while only partial information can be reliably obtained about these states in the form of various biological markers (biomarkers). Tackling this problem requires a multi-faceted and inter-disciplinary approach and involves borrowing techniques from or devising novel ones based in mathematics, optimization, and machine learning.
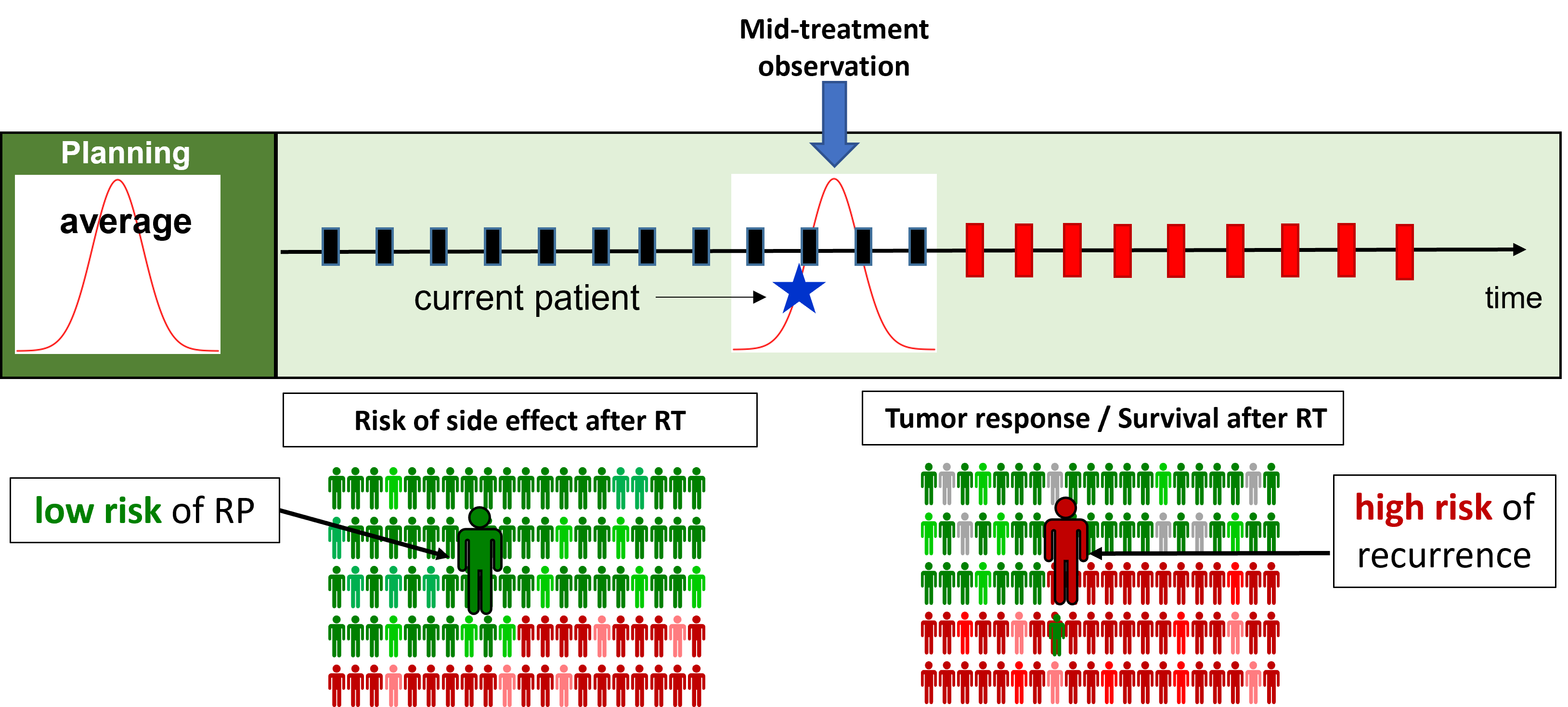
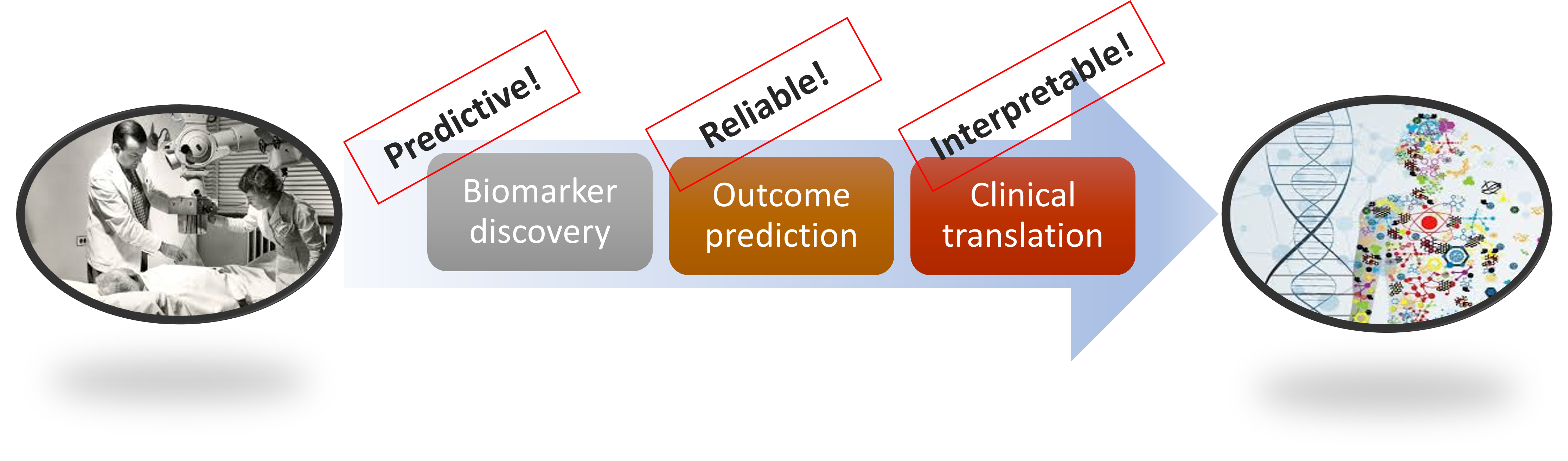
OSRT consists of three interconnected and complimentary steps: (1) Predictive Biomarker Discovery, (2) Interpretable Predictive Modeling, and (3) Adaptive Treatment Personalization. We are actively working to develop effective tools in all three fronts to realize the full potential of OSRT. We heavily rely on advanced methods rooted in Statistics, Machine Learning, and Optimization to perform these steps. In the first one (Biomarker Discovery), we mainly use image processing and advanced statistical and data analytics tools to find novel or re-purpose existing biomarkers of RT response. In the second, state-of-the-art machine learning tools are employed to derive interpretable predictive models of RT response. Finally, the third step involves various forms of optimization methods to address model uncertainty and adapt the treatment plans according to biomarker information and model's predictions. You can find more information about each of these steps in their dedicated sections below.
[1] A. Ajdari, M. Niyazi, N. Nicolay, C. Thieke, R. Jeraj, T. Bortfeld (2019), Towards optimal stopping in radiation therapy, Radiotherapy and Oncology, 137: 96-100.
